INDICATIONS
- Rotator cuff arthropathy
- Severe shoulder arthritis with deficient rotator cuff or bone loss
- Revision shoulder replacement
PREOP
- MRI Scan--Evaluate Rotator Cuff
- CT Scan--Computer Planning
- Medical Clearance with PMD
RECOVERY
- 10 days suture removal
- Three to four weeks sling
- 4-6 months physical therapy 2 x per week.
- Expectation is excellent range of motion and minimal to no pain.
TECHNIQUE
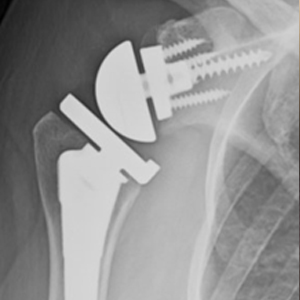
Shoulder ball (humerus) is replaced with a metal stem and plastic tray and shoulder socket (glenoid) is reversed with a metal ball. This geometry allows the shoulder to move without depending on the rotator cuff
DAY OF SURGERY
- Nerve block anesthesia
- 2 hour surgery
- One night in hospital
- 24 hours antibiotics
- No Foley catheter
- PT and OT in hospital
WHEN TO HAVE SURGERY?
- Significant pain
- Loss of motion
- Interrupted sleep
- Poor shoulder function
-
RTSA Implants

-
X-Ray Before

-
X-ray After

Questions?
Email Dr. Gamradt - [javascript protected email address]
[javascript protected email address] Office Phone:











