Overview
The anterior cruciate ligament (ACL) is a main stabilizing ligament of the knee. It prevents abnormal translation and rotation of the tibia with respect to the femur. The ACL is commonly torn during athletics in sports involving cutting or pivoting (e.g. basketball, soccer), but also can be torn in any event that causes an undue rotational force to the knee (twisting injury, collision sports, falls, skiing).
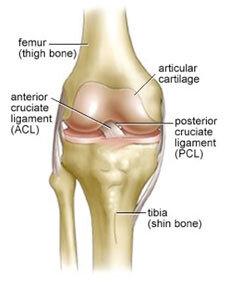
Figure 1: Normal Knee Anatomy. The ACL is stabilizing ligament of the knee that connects the tibia bone to the femur bone.
Many patients who suffer an ACL tear recall the exact moment that the ACL tear happened because they felt a ‘pop’ in the knee and were unable to continue their athletic event. The knee joint commonly swells and is difficult to walk on after injury. A patient with an injured ACL usually is compelled to visit their doctor or emergency room. An untreated ACL injury commonly results in a knee that feels unstable and gives way, especially with sports but sometimes with daily activities as well.
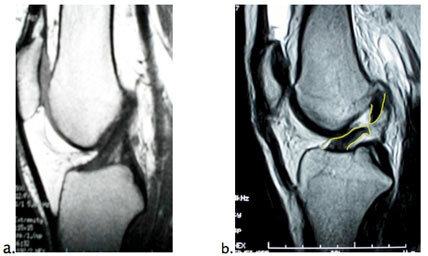
Figure 2:
Diagnosis of ACL Tear
An ACL tear can be reliably diagnosed by a skilled orthopedic physician with history and physical exam. Two tests are used during the physical exam to diagnose a torn ACL. The first is the Lachman exam; during this test the examiner pulls forward on the tibia while stabilizing the femur and abnormal translation is felt. The second is the pivot shift; during this test, the examiner internally rotates the tibia while flexing the knee to demonstrate the rotational instability of the knee with a deficient ACL.
When an ACL injury is suspected, imaging is ordered. X-rays are taken to rule out fracture or malalignment of the knee. An MRI is ordered to confirm the ACL tear but also to evaluate the other ligaments in the knee, cartilage, and meniscus.
Proper diagnosis and management of the injuries associated with ACL tears (e.g. meniscus, cartilage) are critically important for the long term health of the knee. MRI scan can reveal the following injuries associated with an ACL tear:
- Meniscus: The medial and lateral menisci are fibrocartilage cushions between the tibia and femur that act as shock absorbers and distribute stresses placed on the knee joint.’ The meniscus can tear during the trauma that caused the ACL tear as well. Treatment of meniscus tears (repair vs. partial meniscectomy) is based on the size, location, and configuration of the meniscal tear. Depending on these factors the meniscus tear is commonly repaired or excised at the time of ACL reconstruction.
- Articular Cartilage: Cartilage is the smooth gliding surface that coats the end of the femur bone and tibia bone. Damage to articular cartilage is called chondromalacia. The chronic loss of cartilage is called arthritis. Cartilage damage can occur during acute ACL tears or as a result of chronic instability due to a chronic ACL tear.
- MCL: The medial collateral ligament provides stability to the inside aspect of the knee.’ This ligament is commonly injured during an ACL tear as well. Most ACL injuries (Grade 1 and 2 injuries) associated with ACL tears do not require further surgical treatment at the time of ACL reconstruction.
- ACL/PCL/LCL or ACL/PCL/MCL: If the posterior cruciate ligament and medial/lateral collateral ligament is torn in conjunction with the ACL tear, this indicates a higher energy injury. These injuries are termed multi-ligament knee injury and require reconstruction of all injured ligaments.
Once the constellation of injuries to the knee is determined by physical exam, x-ray, and MRI, a plan of treatment is determined. A completely torn ACL will never heal back to it pre-injury ‘normal’ state even after conservative treatment such as rehabilitation.’ The intra-articular nature of the ligament bathes the ends of the injured ACL in joint fluid, preventing primary healing from occurring. For this reason, the ACL is commonly treated surgically with an ACL reconstruction.
Treatment of ACL Tears
An ACL reconstruction surgery is usually recommended in the following situations:
- Athletes who sustain ACL tears almost always require reconstruction of the ACL to return to prior level of competition.
- Symptoms of persistent knee instability and a feeling of giving way in the ACL deficient knee despite rehabilitation.
- Injury to associated structures in the knee (cartilage and meniscus) in the setting of ACL injury is best treated surgically in most cases.
An acutely injured knee with an ACL tear is almost universally treated initially with a course of physical therapy to restore knee range of motion, decrease swelling, and increase strength. Restoration of motion and normal walking after an ACL injury usually takes 3-4 weeks. Once this period of rehabilitation is complete, the knee is ready for reconstruction. Restoration of motion and elimination of most swelling is important prior to surgery to minimize the risk of postoperative stiffness.
ACL tears can be treated without surgery in non-athletic individuals. After completion of rehabilitation, a gradual return to activity is usually tolerated. The rehabilitation program is designed to strengthen the muscles around the knee to prevent instability. Light athletic activities such as cycling and jogging are usually performed pain free. Without ACL reconstruction, however, cutting sports are likely to cause buckling or giving way of the knee which can further injure meniscus and cartilage. Similarly, if daily activities cause instability, it is best to perform surgery to restore stability to the knee to prevent further injury to the cartilage surfaces.
ACL Reconstruction Surgery
Most tears to the ACL are complete ruptures of the ligament at its midpoint. The intra-articular liquid environment of the knee is a poor environment for ligament healing and therefore tears of the ACL do not heal on their own. Similarly suturing the ends of the ligament together has not resulted in successful results due the same poor healing response of the ACL.
Surgery to ‘fix’ the ACL is therefore a reconstruction (ligament replacement) rather than a repair. A reconstruction of the ligament involves placing a new graft across the anatomic site of the normal ACL which runs from the tibia to the femur. A small tunnel is drilled in each bone and a new ligament (the ‘graft’) is brought into the tunnel and is fixed with screws in the anatomic position of the ACL. The operation is performed through small incisions with the aid of an arthroscope (camera within the knee). The type of graft used is specific for each patient and depends both on surgeon preference, patient preference, age, and anatomic factors. Graft types are described as autograft if they come from the patient’s own knee or allograft if they come from cadaver tissue
ACL Graft Options
- Bone-Patellar Tendon-Bone Autograft (BTB): This graft comes from the anterior (front portion) of the knee. A strip of patellar tendon along with two small pieces of bone (bone blocks) is harvested through a small incision. These bone blocks are secured into bone tunnels at the anatomic location where the ACL originates on the femur (the ‘origin’) and the anatomic location where the ACL ends at the tibia (the arcinsertion’).’ BTB autograft has an established track record in young athletes. Advantages included bone to bone healing of the graft, secure fixation and low re-rupture rates. Disadvantages include temporary or rarely permanent pain at the site of harvest and increased pain in the early postoperative course.
- Hamstring Autograft: The hamstring tendons that course along the medial (inner) aspect of the knee can also be used as a graft. These two tendons are called the gracilis and semitendinosus; the tendons are folded over themselves to create a quadrupled hamstring graft. No bone is harvested with the hamstring tendons and therefore, there is less immediate postoperative pain. Traditionally, the downside of hamstring ACL reconstruction is that the fixation of these grafts was not as predictable as the BTB graft, leading to a higher re-rupture rate. Newer fixation devices have largely eliminated this problem and randomized controlled trials have shown relative equivalency between the BTB graft and the hamstring graft. There may be a slight loss of hamstring strength with this graft long-term.
- Allograft: Allograft ACL reconstruction is performed with tissue harvested from organ donors.’ There are many different sources of donor tendons and ligaments that can be used for ACL reconstruction.’ Allograft hamstring, BTB, Achilles tendon, and tibialis anterior are all common sources of allograft tissue used in ACL reconstruction. Advantages of an allograft ACL reconstruction is that no tissue is harvested from the patient’s knee and therefore there is no ‘donor site morbidity.’ Disadvantages include a theoretical risk of disease transmission, infection, or rejection; this risk is exceedingly small due to rigid donor screening and testing as well as irradiation/cleaning of the grafts prior to implantation. Another disadvantage is the possibility of re-rupture in the most high demand, young athletes. Allografts are very commonly used in revision ACL reconstruction and in cases that require the reconstruction of more than one ligament.

Figure 3: Bone Patella Tendon Bone Autograft (BTB)

Figure 4:

Figure 5: Achilles Tendon Allograft
Technical Considerations in ACL Reconstruction
Performing a technically sound ACL reconstruction that recreates the normal anatomy of the native ACL with a securely fixed graft is probably much more important than the type of graft used. ACL surgeons have become increasingly interested in the exact location of the ACL on the tibia and femur (the footprint of the ACL). The tunnels for ACL reconstruction are then drilled as precisely as possible within this footprint on each bone. Some surgeons have even advocated drilling two tunnels in each bone and using two grafts. This is termed a ‘double bundle’ reconstruction. In laboratory studies there is some evidence that a double bundle reconstruction better restores rotational stability to the knee. However, double bundle reconstructions have not outperformed single bundle reconstructions in clinical trials. Furthermore, a double bundle reconstruction comes with the added complexity of four tunnels, four graft fixation devices, and the requirement of using two allograft tendons rather than autograft tissue.
Therefore, at USC we focus on performing an ‘anatomic’ single bundle reconstruction, placing the new ACL graft precisely where it belongs on both the tibia and femur by independently drilling each tunnel in the anatomic footprint of the native ACL.
Effectiveness of ACL Reconstruction
In the hands of an experienced surgeon, arthroscopic ACL reconstruction is very effective at eliminating instability in the knee and returning patients back to high demand sports without pain. The positive effect of the ACL reconstruction is permanent. Greater than 90% of patients are usually satisfied with their surgery and return back to sport. The prognosis of the knee after ACL reconstruction long term depends more on the concomitant injuries to meniscus and cartilage. Over the course of decades, especially in knees with severe cartilage or meniscus injury, arthritis can still develop despite ACL surgery.
Risks of ACL Reconstruction
Theoretical risks of an ACL reconstruction include the following. The surgeon and his or her team will do everything possible to minimize these risks:
- Infection
- Damage to nerves or arteries
- Stiffness
- Pain or weakness at graft donor site
- Scar and peri-incisional numbness
- Rejection/Infection/Disease transmission from allograft (exceedingly low risk)
- Failure or re-rupture of the reconstructed ligament (5%)
- Failure to return to previous level of sport
- Reoperation
- Anesthesia risk
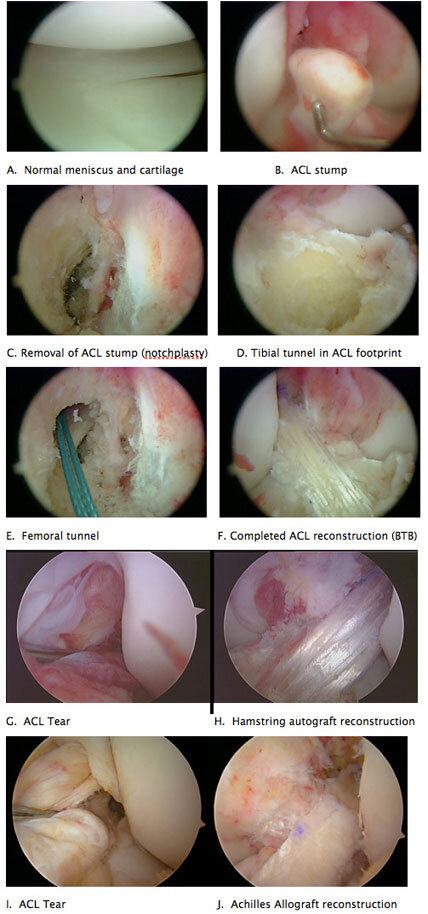
Figure 6: Arthroscopic pictures of an ACL reconstruction

Figure 7
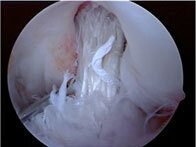
Figure 8: Vertical and anterior graft.

Figure 9: Revised with Achilles Allograft

Figure 10: Absent ACL after reconstruction.

Figure 11: Revision with BTB autograft
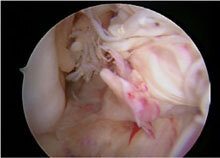
Figure 12: Well-functioning graft with traumatic re-rupture.
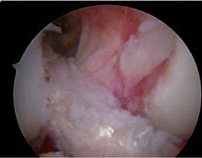
Figure 13: Revised with Allograft
What to Expect
ACL reconstruction is performed as outpatient surgery. Surgery takes 1.5 to 2 hours to complete. General and/or regional anesthesia is required. After the surgery sterile bandages are applied as well as a hinged knee brace and a cold-therapy device (Cryo-cuff). The patient can leave the same day on crutches to limit weight bearing on the leg.
Pain medications (Percocet) and an anti-inflammatory (Naprosyn) are provided. Prolonged sitting/standing/walking are avoided for the first 7 days. Patients with desk jobs can return to work after about 1 week. To shower, the leg is covered with a plastic bag until the wounds are healed (7-10 days). Crutches and the brace are used for 3-4 weeks depending on the type of graft and concomitant injuries to the knee. Gentle range of motion and strengthening exercises begin immediately and formal physical therapy starts 3-5 days after surgery.
Rehabilitation
Rehabilitation after ACL reconstruction is lengthy. In general it follows the outline below, although there are certain patients who progress more quickly or more slowly. The rate limiting factor is the healing of the graft within the knee. The graft is probably not ‘incorporated’ into the knee until 6 months.
- 0-3 weeks: Crutches, brace, range of motion as tolerated, gentle quad strengthening
- 3-8 weeks: Restore full range of motion, decrease swelling, improve strength, normalize walking
- 8-16 weeks: Extensive strengthening of the leg
- 16-18 weeks: Jogging on flat ground permitted, continue strengthening
- 20-24 weeks: Agility drills added, sport specific training
- 6-9 months: Return to sport allowed provided range of motion and strength are close to normal.
Adolescent/Pediatric ACL Reconstruction
Because the growth plates of the femur and tibia are open and the child has significant growth left in the leg, conventional ACL reconstruction can result in a growth disturbance to the leg. For this reason, special consideration is paid to the age of the patient, activity level of the patient, and amount of growth remaining.
In addition, nonoperative treatment and bracing can be considered to allow young patients to get closer to skeletal maturity before ACL reconstruction is performed.
The pediatric ACL/adolescent ACL patient is commonly divided into three groups based on amount of growth left in the affected knee:
- Skeletally immature (10-12yo Females, 11-13yo Males). In these cases, a large amount of bone growth remains and therefore, ACL reconstruction if recommended proceeds with a technique that avoids the femoral and tibial growth plates altogether. This can be accomplished with an ‘over the top, over the front’ hamstring reconstruction or by an iliotibial band reconstruction.
- Close to skeletal maturity (13-14yo Females, 14-15yo Males). In this group, less growth remains and crossing the growth plate with a standard hamstring ACL reconstruction is effective.
- Skeletally mature (>15yo Females, >16yo Males). These patients have little or no growth remaining at the knee and often can be reconstructed in a manner similar to adults.
Figure 7: Hamstring autograft reconstruction in 14-year-old female
Revision ACL Reconstruction
A knee that remains persistently unstable after ACL reconstruction or returns to an unstable state after an injury is considered a failed ACL reconstruction. There are multiple different reasons why an ACL reconstruction can fail. They are commonly divided into three categories:
- TECHNICAL FAILURE: A poorly performed ACL reconstruction is usually the result of tunnel malposition on the femur or tibia or a fixation failure of the graft. Therefore, the graft does not reproduce normal anatomy and the knee remains unstable. These patients often state that the knee never felt ‘right’ after surgery and never returned to previous level of sport.
- BIOLOGIC FAILURE: A graft that fails to heal or an allograft that is rejected is termed a biologic failure. Similarly, these patients often state that the knee never felt ‘right’ after surgery and never returned to previous level of sport.
- TRAUMATIC FAILURE: A well-functioning graft that re-ruptures is termed a traumatic rupture. The patient will often report and uneventful recovery and return to sport and a knee that felt good. A new injury can re-rupture the well-functioning graft in about 5% of ACL surgeries.
Revision ACL reconstruction is less predictable and successful in comparison to primary ACL reconstruction. In general, revisions are more successful when instability of the knee is the main complaint rather than pain in the knee. Revision surgery is individualized and requires specialized equipment; graft choice is usually allograft. Prior to revision ACL surgery, your surgeon will order x-rays, repeat MRI, and possibly CT scan for preoperative planning. Also, your previous operative report will be required for planning surgery. On occasion, the surgery will need to be performed in two stages. Rehabilitation after revision ACL surgery follows a slightly slower timeline than in primary ACL surgery.











